CCIM Connections
The Official Publication of The CCIM Institute
Image

Fall 2024
Cover Story
Supreme Court Overturns Chevron Doctrine, Reshaping CRE Regulation
Read ArticleImage

The Latest Trending Articles
Featured Articles by Issue
Stay Up to Date on All Issues
Hero image
Intro Text
Bringing Success and Strength to The CCIM Institute
Hero image

Intro Text
Making Deals - Spring 2024
Intro Text
Driving The CCIM Institute's Growth
Hero image
Intro Text
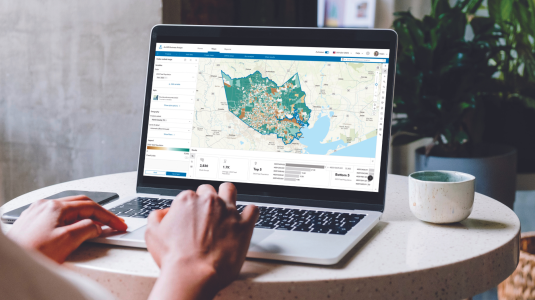
Site To Do Business is commercial real estate's most advanced digital toolkit providing essential data components and marketing tools to give your audience a broader perspective on today's market.